
Hereditary hemorrhagic telangiectasia (HHT) is an inherited autosomal dominant disorder that leads to abnormal formation of blood vessels throughout the body. Patient symptoms primarily consist of bleeding from various mucosal surfaces to more severe or life-threatening hemorrhage in the lung, brain, or liver.
The physical signs of HHT consist primarily of telangiectasias (dilated capillaries) on mucosal and cutaneous skin surfaces and arterio-venous malformations (AVMs) in various internal organs. The telangiectasias tend to spontaneously rupture, most commonly resulting in nasal or gastrointestinal bleeding.
A clinical diagnosis of HHT is based on the Curaçao Criteria, which involves a combination of epistaxis, telangiectasias, visceral lesions (AVMs), and a family history of a first-degree relative with HHT. Symptoms are age-dependent and gradually emerge over time. By age 20, more than 75% of patients with HHT have developed recurrent epistaxis, which is the leading cause of morbidity in HHT.
NOSE HHT
The NOSE HHT provides clinicians with a validated measurement of physical, functional, and emotional consequences of HHT-associated epistaxis and can be used as an outcome measure in future epistaxis clinical trials. The 29-item NOSE HHT, with total scores ranging continuously from 0-4, proved to be internally consistent, highly correlated with epistaxis severity, and responsive to change. It had a high test-retest reliability and a minimal clinically important difference of 0.46 points.
Nasal Outcome Score for Epistaxis in Hemorrhagic Telangiectasia (NOSE HHT) »
Epistaxis Severity & Treatment
Hereditary hemorrhagic telangiectasia (HHT) is an autosomal dominant inherited disorder that progressively manifests with telangiectasias, mucosal bleeding, and possibly solid organ hemorrhage within the first few decades of life. Epistaxis with varying levels of severity is the most common presentation of the disease. To date, a variety of medical, procedural, and surgical treatments have been used to treat epistaxis in HHT, both acutely and chronically. No standard of care has been agreed upon, as there is a wide range of efficacy and safety concerns with the various treatment options.
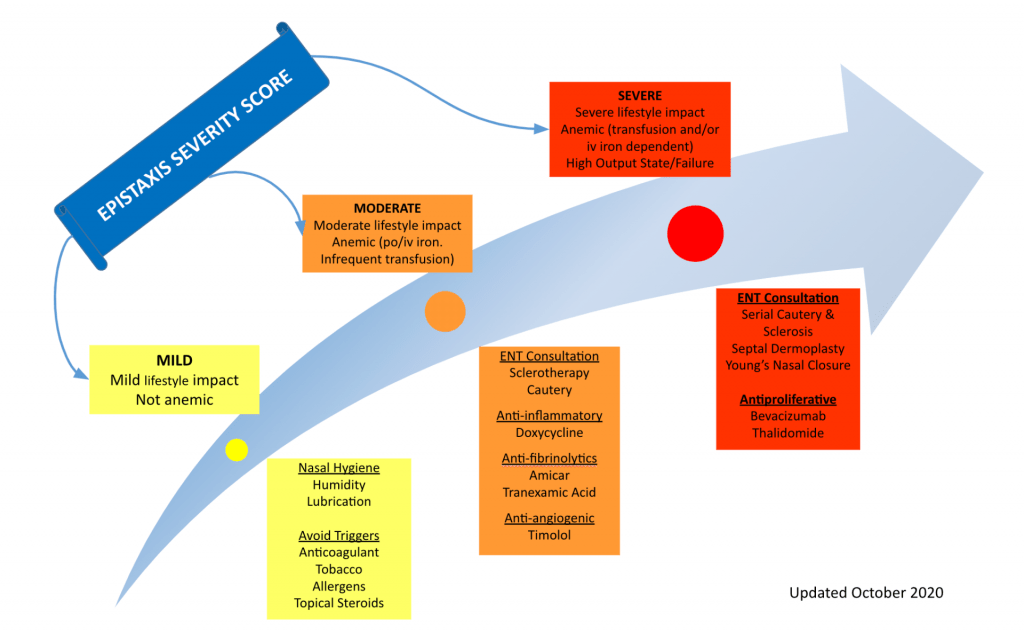
Figure: Standard Medical Management for HHT‐Associated Epistaxis Based on Epistaxis Severity Score
HHT Publications
Treatments For Refractory HHT-Associated Epistaxis by Jay Piccirillo, MD »
Efficacy of Timolol in a Novel Intranasal Thermosensitive Gel for Hereditary Hemorrhagic Telangiectasia-Associated Epistaxis: A Randomized Clinical Trial.
Objective of this clinical trial conducted was at Washington University Department of Otolaryngology-Head and Neck Surgery was to determine the efficacy and safety of an intranasal timolol thermosensitive gel vs placebo thermosensitive gel in treating HHT-associated epistaxis. This double-blind, placebo-controlled randomized clinical trial was conducted from October 29, 2019, to May 20, 2020.
A total of 27 patients with HHT and moderate-to-severe epistaxis were recruited and included in this study. The intervention consisted of novel thermosensitive intranasal timolol (0.1%) gel vs placebo thermosensitive gel applied twice daily to each nostril for 8 weeks. Of the 27 participants randomized (median [range] age, 55 [20-76] years; 14 women [52%]; 25 White [93%]), a total of 23 patients with HHT completed the primary outcome measure.
Within the timolol gel and placebo gel groups, respectively, the median change (range) in ESS was 2.32 (0.22 to 5.97) vs 1.96 (-0.91 to 5.98), and 9 of 11 (82%) vs 9 of 12 (75%) participants experienced a clinically meaningful improvement in ESS. Twenty-two of the 23 participants (96%) reported improvement via the Clinical Global Impression-Improvement score, with 81% vs 58% of participants reporting reduced severity of epistaxis in the timolol vs placebo group, respectively.
Of participants completing the Nasal Outcome Score for Epistaxis in HHT at follow-up visit, 7 of 10 (70%) in the timolol group achieved a clinically important difference vs 5 of 10 (50%) in the placebo group. In conclusion, thermosensitive gel, alone or in combination with timolol, was highly effective in reducing HHT-associated epistaxis. The timolol group had greater improvement in epistaxis and quality of life than the placebo group, but effect estimates were imprecise, and no definitive conclusions on the superiority of timolol can be drawn. Physicians treating patients with HHT-associated epistaxis should consider a thermosensitive gel (with or without timolol) for their patients.
Peterson AM, Lee JJ, Kallogjeri D, Schneider JS, Chakinala MM, Piccirillo JF. Efficacy of Timolol in a Novel Intranasal Thermosensitive Gel for Hereditary Hemorrhagic Telangiectasia-Associated Epistaxis: A Randomized Clinical Trial. JAMA Otolaryngol Head Neck Surg. 2020.